Brazil Healthcare Claims Management Market
Brazil Healthcare Claims Management Market Size, Share, By Product (Medical Billing, Claims Processing), By Component (Services, Software), By Solution Type (Integrated Solutions, Standalone Solutions), By Delivery Mode (On-premises, Cloud-based, Web-based), By End User (Healthcare Payers, Healthcare Providers, and Others), Brazil Healthcare Claims Management Market Insights, Industry Trend, Forecasts to 2035
Report Overview
Table of Contents
Brazil Healthcare Claims Management Market Size Insights Forecasts to 2035
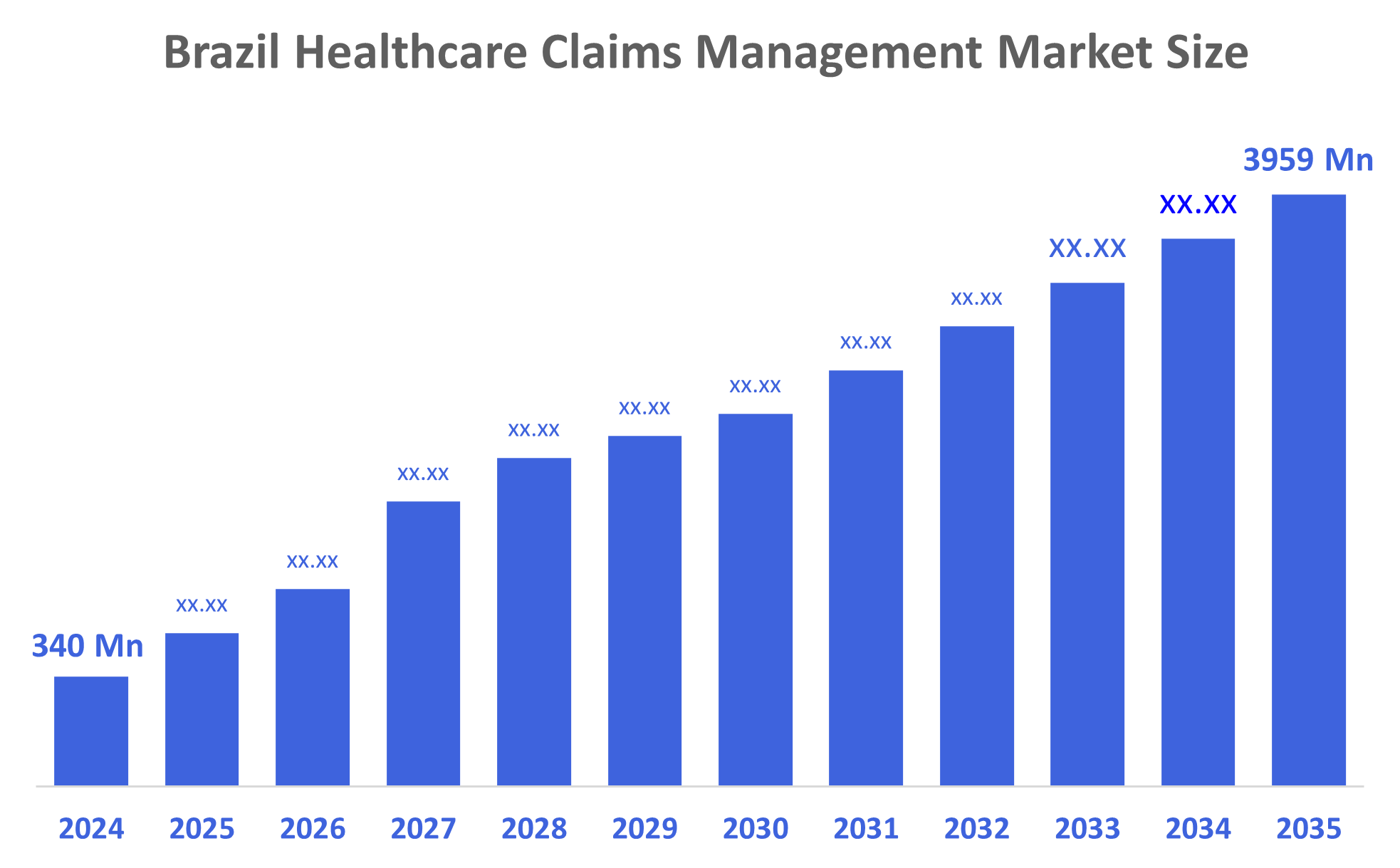
- Brazil Healthcare Claims Management Market Size 2024: USD 340 Mn
- Brazil Healthcare Claims Management Market Size 2035: USD 3959 Mn
- Brazil Healthcare Claims Management Market CAGR 2024: 25%
- Brazil Healthcare Claims Management Market Segments: product, Component, Solution Type, Delivery Mode, and End User
Healthcare claims management is essentially the organization of insurance paperwork where one creates, sends, reviews, and follows up on requests for money due to hospital visits. It is a series of activities that include patient eligibility verification, disease and treatment coding, adhering to the payer regulations, denial management, and revenue cycle efficiency optimization for healthcare providers and payers. Besides, Brazil's healthcare claims management market is expanding as a result of the higher demand for healthcare services, government digital health initiatives, increased utilization of automated and cloud-based claims solutions, AI integration for efficiency and fraud detection, and more extensive private health insurance coverage that generates the need for streamlined, compliant claims processing systems.
The government of Brazil supports healthcare claims management through digital health policies that facilitate interoperability, electronic health records, and data integration across different systems. The regulatory authorities, such as ANS and SUSEP, not only standardize billing, compliance, data protection, and transparency but also promote the use of automation, which leads to less fraud, gives faster reimbursements, and efficient claims processing in both public and private sectors of healthcare.
Brazil Healthcare Claims Management Market Size is turning to AI and machine learning to achieve automated adjudication, predictive analytics, and deepened fraud detection. The use of Robotic Process Automation (RPA) in routine work is therefore very efficient as it reduces the number of mistakes and the waiting time. The cloud, based solutions have made it possible for healthcare providers to expand their services and have real-time communication with EHRs, while natural language processing (NLP) helps in getting the data from the unstructured one. Blockchain
Market Dynamics of the Brazil Healthcare Claims Management Market:
Brazil Healthcare Claims Management Market Size is driven by rising demand for medical services, increasing the need for efficient claims processing. Adoption of digital technologies like AI, machine learning, robotic process automation, and electronic health records improves accuracy, reduces errors, and lowers costs. Government policies promoting data integration, interoperability, and compliance support modernization. Additionally, efforts to prevent fraud, streamline billing, and enhance patient experience further propel growth in both public and private healthcare sectors.
Brazil Healthcare Claims Management Market Size faces restraints from high technology implementation costs, a shortage of skilled professionals, and resistance to change among providers. Complex regulations, data privacy concerns, and fragmented healthcare infrastructure also limit seamless integration, while low digital literacy in some regions slows adoption and overall market growth.
The Brazil Healthcare Claims Management Market Size offers significant opportunities for growth. Increasing adoption of digital health solutions, AI, machine learning, and robotic process automation can further improve efficiency, accuracy, and cost savings in claims processing. Expansion of private healthcare and insurance coverage creates higher demand for streamlined claim workflows. Government initiatives supporting interoperability, data standardization, and regulatory compliance encourage modernization. Additionally, telemedicine integration, advanced analytics, and fraud detection technologies provide opportunities for innovation. Collaboration between providers, payers, and technology vendors can drive market expansion and improved patient satisfaction.
Market Segmentation
The Brazil Healthcare Claims Management Market share is classified into product, component, solution type, delivery mode, and end user.
By Product:
The Brazil Healthcare Claims Management Market Size is divided by product into medical billing and claims processing. Among these, the claims processing segment dominated the share in 2024 and is anticipated to grow at a remarkable CAGR during the forecast period. The claims processing segment dominates due to the growing need for efficient, accurate, and automated claim handling. Rising healthcare demand, coupled with the adoption of AI, machine learning, robotic process automation, and electronic health records, helps reduce errors, prevent fraud, and speed reimbursements. These technological and operational advantages make claims processing more critical and widely adopted than traditional medical billing, driving its leading position in the market.
By Component:
The Brazil Healthcare Claims Management Market Size is divided by component into services and software. Among these, the services segment dominated the share in 2024 and is anticipated to grow at a remarkable CAGR during the forecast period. The services segment dominates because many providers and insurers prefer outsourced or managed solutions to handle complex claims workflows efficiently. Services cover claim processing, denial management, compliance support, and operational assistance, reducing internal workload and errors. While software is important, service providers deliver end-to-end, customized solutions that ensure faster reimbursements, regulatory adherence, and improved patient satisfaction, making this segment more widely adopted and valuable than standalone software.
Solution Type:
The Brazil Healthcare Claims Management Market Size is divided by solution type into integrated solutions and standalone solutions. Among these, the integrated solutions segment dominated the share in 2024 and is anticipated to grow at a remarkable CAGR during the forecast period. Integrated solutions dominate because they combine multiple tasks like claims processing, billing, and eligibility checks in one platform. This makes work faster, easier, and more accurate. Providers and insurers can process claims quickly, reduce errors, and follow regulations, so integrated solutions are preferred over standalone systems.
Delivery Mode:
The Brazil Healthcare Claims Management Market Size is divided by delivery mode into on-premises, cloud-based, and web-based. Among these, the cloud-based segment dominated the share in 2024 and is anticipated to grow at a remarkable CAGR during the forecast period. The dominance of cloud-based solutions is due to their flexibility, scalability, and cost-effectiveness. Cloud platforms allow healthcare providers and insurers to access real-time data remotely, integrate easily with electronic health records, and streamline claims processing. They reduce the need for on-site IT infrastructure, lower maintenance costs, and provide automatic updates. These advantages improve efficiency, accuracy, and compliance, making cloud-based delivery the preferred choice over on-premises and web-based solutions in the market.
End User:
The Brazil Healthcare Claims Management Market Size is divided by end user into healthcare payers, healthcare providers, and others. Among these, the healthcare providers segment dominated the share in 2024 and is anticipated to grow at a remarkable CAGR during the forecast period. The dominance of healthcare providers in Brazil’s healthcare claims management market is driven by their high volume of medical services and claims, which require accurate, timely, and compliant processing. Hospitals, clinics, and diagnostic centers face pressure to reduce errors, prevent fraud, and ensure faster reimbursements. Adoption of technologies like AI, robotic process automation, and electronic health records helps providers streamline workflows and improve efficiency. Consequently, providers represent the largest end-user segment, generating the highest demand for claims management solutions and services.
Competitive Analysis:
The report offers the appropriate analysis of the key organisations/companies involved within the Brazil Healthcare Claims Management Market Size, along with a comparative evaluation primarily based on their product offering, business overviews, geographic presence, enterprise strategies, segment market share, and SWOT analysis. The report also provides an elaborative analysis focusing on the current news and developments of the companies, which includes product development, innovations, joint ventures, partnerships, mergers & acquisitions, strategic alliances, and others. This allows for the evaluation of the overall competition within the market.
Top Key Companies in Brazil Healthcare Claims Management Market:
- Bradesco Saúde / Bradesco Seguros
- Amil (UnitedHealth Group)
- Sinistro Facil
- Guardian
- BM Contas Médicas
- FAT
- IntuitiveCare
- Accenture
- Others
Recent Developments in Brazil Healthcare Claims Management Market:
In March 2025, Optum launched Integrity One, an AI-based revenue-cycle platform that raised coder productivity by 20% during pilot implementations.
In April 2023, Google Cloud introduced a new AI-enabled Claims Acceleration Suite that streamlines prior authorization and claims processing for health insurance. The solution, which leverages the newly developed Claims Data Activator, will assist health plans and providers in reducing administrative burdens and costs by transforming unstructured data into structured data, enabling experts to make quicker, more informed decisions to improve patient care.
Key Target Audience
- Market Players
- Investors
- End-users
- Government Authorities
- Consulting and Research Firm
- Venture capitalists
- Value-Added Resellers (VARs)
Market Segment
This study forecasts revenue at the Brazil, regional, and country levels from 2020 to 2035. Decisions Advisors has segmented theBrazil Healthcare Claims Management Market Size based on the below-mentioned segments:
Brazil Healthcare Claims Management Market, By Product
- Medical Billing
- Claims Processing
Brazil Healthcare Claims Management Market, By Component
- Services
- Software
Brazil Healthcare Claims Management Market, By Solution Type
- Integrated Solutions
- Standalone Solutions
Brazil Healthcare Claims Management Market, By Delivery Mode
- On-premises
- Cloud-based
- Web-based
Brazil Healthcare Claims Management Market, By End User
- Healthcare Payers
- Healthcare Providers
- Others
FAQ
Q1: How do healthcare claims management systems benefit Brazilian providers?
- They streamline claim submissions, reduce manual errors, speed reimbursements, and provide real-time insights into claim status, improving operational efficiency and financial planning.
Q2: Why are cloud-based solutions preferred?
- Cloud platforms offer remote accessibility, scalability, automatic updates, and easier integration with electronic health records, which enhances efficiency and lowers IT maintenance costs.
Q3: How does AI impact claims management?
- AI automates claim adjudication, detects fraudulent patterns, analyzes unstructured data, and predicts potential denials, enabling faster and more accurate decisions.
Q4: What role does government policy play?
- Policies supporting digital health, interoperability, and compliance encourage modernization, data security, and adoption of advanced claims processing systems.
Q5: Who drives demand for claims management solutions?
- Healthcare providers dominate due to high claim volumes, the need for accurate reimbursements, and operational efficiency.
Q6: What are the current market opportunities?
- Opportunities include AI-driven automation, telemedicine integration, fraud prevention, advanced analytics, and partnerships between payers, providers, and tech companies.
Q7: What are recent innovations?
- Google Cloud’s AI-enabled Claims Acceleration Suite and MedLM models improve automation, structured data processing, and faster claim adjudication.
Q8: What challenges limit growth?
- High costs, shortage of skilled professionals, fragmented infrastructure, resistance to digital adoption, and complex regulatory compliance remain key challenges.
Check Licence
Choose the plan that fits you best: Single User, Multi-User, or Enterprise solutions tailored for your needs.
We Have You Covered
- 24/7 Analyst Support
- Clients Across the Globe
- Tailored Insights
- Technology Tracking
- Competitive Intelligence
- Custom Research
- Syndicated Market Studies
- Market Overview
- Market Segmentation
- Growth Drivers
- Market Opportunities
- Regulatory Insights
- Innovation & Sustainability
Report Details
| Scope | Country |
| Pages | 220 |
| Delivery | PDF & Excel via Email |
| Language | English |
| Release | Dec 2025 |
| Access | Download from this page |
